A Smart Remote Monitoring System for Prenatal Care in Rural Areas
Main Article Content
Abstract
The complications in maternity especially the women lives in rural sector can be reduced through regular monitoring of their vitals like blood pressure, SpO2 and fetal growth. The internet of things (IoT) is the modern technology bridges the gap between the traditional clinical setting with its consumers as well promotes the telemedicine industry into great levels of accessing proactive healthcare facilities. The predominant aim of this work is to bring a remote monitoring device which assesses the significant health indicators of the pregnant women and their fetus status cost effectively. In order to build such kit, the biosensors like heart rate, SpO2, pressure, temperature and load cell which gives the weight of the fetus are integrated into Arudino board. The sensor readings are processed through ThingSpeak. The timely medical attention is proposed upon observing abnormal physiological vitals of the women which is implemented through a buzzer system in this device. Like such devices in realism help to predict the pregnancy risk and decrease the mortality rate.
Article Details
References
G. Robbers, J. P. Vogel, G. Mola, J. Bolgna and C. S. E. Homer, “Maternal and newborn health indicators in Papua New Guinea – 2008–2018,” Sexual and Reproductive Health Matters, vol. 27, no. 1, pp. 52-68, 2019, doi: 10.1080/26410397.2019.1686199.
P. J. Saturno-Hernández, I. M. Nicolás, E. M. Zegbe, M. F. Elorriaga and O. P. Verástegui, “Indicators for monitoring maternal and neonatal quality care: a systematic review,” BMC Pregnancy and Childbirth, vol. 19, no. 25, pp. 11, 2019, doi: 10.1186/s12884-019-2173-2 .
K. S. Vora, D. V. Mavalankar, K.V. Ramani, M. Upadhyaya, B. Sharma, S. Iyengar, V. Gupta, and K. Iyengar, “Maternal Health Situation in India: A Case Study,” Journal of Health, Population and Nutrition, vol. 27, no. 2, pp.184–201, April 2009, doi: 10.3329/jhpn.v27i2.3363.
A. A. Bhattacharya, N. Umar, A. Audu, H. Felix, E. Allen, J. R. M. Schellenberg and T. Marchant, “Quality of routine facility data for monitoring priority maternal and newborn indicators in DHIS2: A case study from Gombe State, Nigeria,” PLoS ONE, vol. 14, no. 1, pp. 1-21, January 2019, https://doi.org/10.1371/journal.pone.0211265.
Barbara Madaj,Helen Smith, Matthews Mathai, Nathalie Roosb and Nynke van den Broek, “Developing global indicators for quality of maternal and newborn care: a feasibility assessment,” Bull World Health Organ, vol. 95, pp. 445-452, March 2017.
B. Mostafavi, “Rural Women at Higher Risk of Life-Threatening Pregnancy Complications,” 2019, https://ihpi.umich.edu/news/rural-women-higher-risk-life-threatening-pregnancy-complications.
Vanessa Brizuela, Hannah H Leslie, Jigyasa Sharma, Ana Langer and Özge Tunçalp, “Measuring quality of care for all women and newborns: how do we know if we are doing it right? A review of facility assessment tools,” Lancet Glob Health, vol. 7, pp. 1-9, March 2019, https://doi.org/10.1016/S2214-109X(19)30033-6.
A. C. Moran, K. Kerber, D. Sitrin, T. Guenther, C. S. Morrissey, H. Newby, J. Fishel, P. S. Yoder, Z. Hill and J. E. Lawn, “Measuring Coverage in MNCH: Indicators for Global Tracking of Newborn Care,” PLOS Medicine, vol. 10, no. 5, pp. 1-9, May 2013, doi: 10.1371/journal.pmed.1001415 .
A. E. Sprague, S. I. Dunn, D. B. Fell, J. Harrold, M. C. Walker, S. Kelly and G. N. Smith, “Measuring Quality in Maternal-Newborn Care: Developing a Clinical Dashboard,” J Obstet Gynaecol Can, vol. 35, no. 1, pp. 29-38, 2013, doi: 10.1016/s1701-2163(15)31045-8. .
A. P. Zielinska, E. Mullins and C. Lees, “The feasibility of multimodality remote monitoring of maternal physiology during pregnancy,” Medicine, vol. 101, no. 26, pp. 1-8, April 2022, doi: 10.1097/MD.0000000000029566..
C. Wakefield, L. Yao, S. Self and M. G. Frasch, “Wearable technology for health monitoring during pregnancy: an observational cross?sectional survey study,” Archives of Gynecology and Obstetrics, pp. 1-6, July 2022, doi: 10.1007/s00404-022-06705-y.
M. N. Sachin, B. Gagandeep, S. A. Nagaraja, B. O. Narendra and R. Naseer, “Smart Prenatal Health Care Monitoring System for Pregnancy Women in Rural Areas using IoT,” International Research Journal of Engineering and Technology, vol. 9, no. 7, pp. 1781-1785, July 2022.
Dennis Ryu, Dong Hyun Kim, Joan T. Price, Jong Yoon Lee, Ha Uk Chung, Emily Allen, Jessica R. Walter, Hyoyoung Jeong, Jingyue Cao, Elena Kulikova, Hajar Abu-Zayed, Rachel Lee, Knute L. Martell, Michael Zhang, Brianna R. Kampmeier, Marc Hill, JooHee Lee, Edward Kim, Yerim Park, Hokyung Jang, Hany Araf, Claire Liu, Maureen Chisembele, Bellington Vwalika, Ntazana Sindano, M. Bridget Spelke, Amy S. Paller, Ashish Premkumar, William A. Grobman, Jeffrey S. A. Stringer, John A. Rogers and Shuai Xud, “Comprehensive pregnancy monitoring with a network of wireless, soft, and flexible sensors in high- and low-resource health settings,” The Proceedings of the National Academy of Sciences (PNAS), vol. 118, no. 20, pp. 1-11, 2021, https://doi.org/10.1073/pnas.2100466118.
K. Revathi and A. Samydurai, “Exploiting the Interdependence of Electrocardiography (ECG) with Other Physiological Parameters of Human Body in Remote Monitoring System,” International Journal of Innovative Technology and Exploring Engineering, vol. 8, no. 10, pp. 1057-1062, August 2019, DOI: 10.35940/ijitee.G5929.0881019.
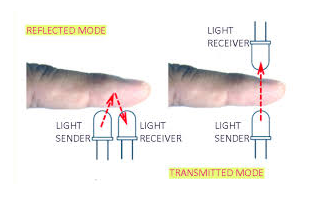
K. Revathi, T. Tamilselvi, G. Gomathi and R. Divya, “IoT Based Pulse Oximeter for Remote Health Assessment: Design, Challenges and Futuristic Scope,” International Journal of Electrical and Electronics Research, vol. 10, no. 3, pp. 557-563, September 2022, https://doi.org/10.37391/IJEER.100325.
Fatemeh Sarhaddi, Iman Azimi, Sina Labbaf, Hannakaisa Niela-Vilén, Nikil Dutt, Anna Axelin, Pasi Liljeberg and Amir M. Rahmani, “Long-Term IoT-Based Maternal Monitoring: System Design and Evaluation,” Sensors, vol. 21, pp. 1-21, 2021, doi: 10.3390/s21072281.
S. A. Z. Hassan and A. M. Eassa, “A Proposed Architecture for Smart Home Systems Based on IoT, Context-awareness and Cloud Computing,” International Journal of Advanced Computer Science and Applications, vol.13, no. 6, pp. 89-96, 2022, (DOI) : 10.14569/IJACSA.2022.0130612 .
S. Veena and D. John Aravindhar, “Remote Monitoring System for the Detection of Prenatal Risk in a Pregnant Woman,” Wireless Personal Communications, pp. 1-14, July 2021, https://doi.org/10.1007/s11277-021-08249-x.
S.Shiny Amala and S.Mythili, “IoT Based Health Care Monitoring System for Rural Pregnant Women,” International Journal of Pure and Applied Mathematics, vol. 119, no. 15, pp.837-843, 2018.
Saniya Ansari and M.B. Ansari, “Smart Health Monitoring System for Pregnant Women,” International Journal of Engineering and Advanced Technology , vol. 9, no. 4, pp. 923-926, April 2020, DOI: 10.35940/ijeat.D7114.049420 .
A. O. Alokaily, G. Almeteb, R. Althabiti and S. S. Alshahrani, “Towards Home-based Therapy: The Development of a Low-cost IoT-based Transcranial Direct Current Stimulation System,” International Journal of Advanced Computer Science and Applications, vol. 13, no. 10, pp. 142-146, 2022.
Yajie Liu, “Smart Greenhouse Monitoring and Controlling based on NodeMCU,” International Journal of Advanced Computer Science and Applications, vol. 13, no. 9. pp. 597-600, 2022.